An introduction to why Thermotherapy works
Homeostasis is complex
Thermotherapy takes advantage of your body’s response to heat and cold as it attempts to maintain homeostasis.1
Wikipedia defines homeostasis as:
“the state of steady internal, physical, and chemical conditions maintained by living systems. This is the condition of optimal functioning for the organism and includes many variables, such as body temperature and fluid balance, being kept within certain pre-set limits (homeostatic range).”
This is a very complex process. The Wikipedia article goes on to list 17 different controls of the many variables. Thermotherapy affects most of these controls in some way. The ones that we actively aim at working with are, temperature (both core and local) and blood pressure.
With local thermotherapy, the nervous system has always been used extensively to produce localised effects.1
Homeostasis set points vary, as the Wikipedia article explains. Homeostasis fails in conditions such as type 1 diabetes, diabetes insipidus and thyroid disease. Also, as we get older our homeostasis becomes unstable, and in chronic disease, homeostasis adjusts to temporarily compensate for the disease symptoms.
Circulation is more complex than we expected
Traditionally we knew, by simply observing changes in skin colour and local swelling, that local and whole-body thermotherapy could be used to finely control the circulation of blood and lymph. Even the circulation in internal organs can be controlled by local thermal treatments that utilise spinal reflexes and closed-system hydrostatic principles.1
Recently the interstitium, another fluid system, has been studied because it is where many diseases originate or develop. According to Wikipedia these include diseases of the lungs, heart and kidney, as well as cancer and systemic autoimmune diseases.
The Wikipedia article explains that the interstitium is a fluid-filled honeycomb space that surrounds all the parts of our body. It makes up about 12% of our body weight, while our blood plasma makes up about 5%.2 Even though we don’t know for sure I’m confident that thermotherapy does affect the interstitium, not least because diseases that involve the interstitium such as Alzheimer’s3 and heart failure,4 also respond to thermotherapy.
On the microscopic level why thermotherapy works, is that it promotes angiogenesis. This is the growth of new blood vessels, needed to relieve such diseases as sarcopenia (muscle wasting in old age), congestive heart failure and chronic obstructive airway disease.5 In congestive heart failure thermotherapy improves the health and function of the endothelial cells that line our blood vessels.6
Heat shock proteins (HSPs) produced during body heating, are important in both angiogenesis and endothelial health. Wikipedia has an introduction to HSPs to give you some idea of these amazing proteins, but HSPs are only one of several protein families, as well as stem cells, that are influenced by thermotherapy.6
The Immune System is really complex
Heating the body has traditionally been used for infective illnesses, we are only recently finding out why it’s effective.
Fever therapy, or hyperthermia, where the body temperature is raised slightly, inhibits many viruses and bacteria, while at the same time stimulating our immune system. White blood cells, particularly monocytes, natural killer cells, and other lymphocytes become more active, the hormones that limit the immune system are suppressed and most immune cell production increases. Heat shock proteins are released and protect the immune cells, assist in antibody production, and generally make sure the body is in the best condition to fight infections.7
Why thermotherapy works in chronic conditions is usually mainly because of heat treatment but in acute infections, we often add short cold treatments to the heating. This increases the production of white blood cells, especially granulocytes and natural killer cells and stimulates them to greater activity. Interleukin-6 levels also increase.8
The result, in my experience, is that three daily treatments of “long heat, short cold” therapy, early in an acute fever are usually enough to resolve the fever. This fits the timeline in the figure below.
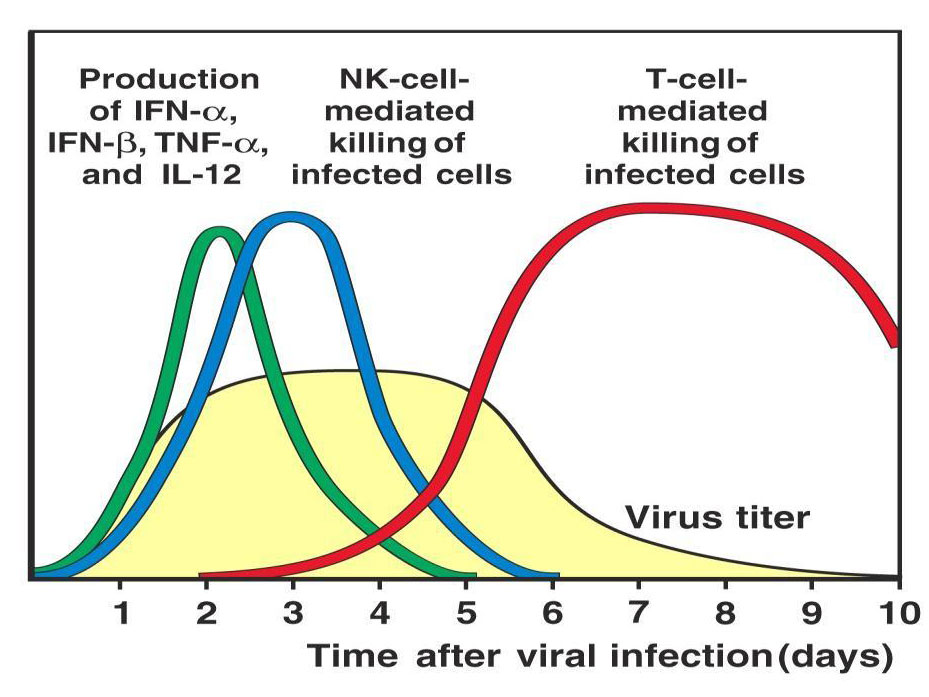
Tracking the immune response to influenza infection (Immunobiology, 6th edition by Charles Janeway, 2005).
It takes about 2 days for the symptoms of flu to appear (which is when we’d start treatment) so if the treatment increases the NK activity and the IL-6 promotes antibody production, day 3 of treatment would be about day 5 since infection, just when virus numbers begins to drop. But I suspect the treatment speeds the process as well as augments it.
Influenza and COVID-19
With COVID-19 the immune response is often suppressed in the early stages in the same areas that thermotherapy stimulates.9 COVID symptoms appear much later too, between 5 and 14 days, so it’s essential to get onto treatment immediately the symptoms are felt.
The most research on the immune system and thermotherapy are where “moderate” hyperthermia (heating the body to 40-44°C for two hours or more), or local heating, are used in conjunction with radiation or chemotherapy to treat cancer.10 These body temperatures are beyond what is achieved in the sort of thermotherapy I use but the effects on the immune system are not that much different. It makes me wonder if frequent lower-temperature treatments might achieve similar results to the more heroic, but less frequent treatment used in the cancer treatments.
A good introduction to the immune system in relation to “hyperthermia” and cancer, is contained in this article from 2012, Old and new facts about hyperthermia-induced modulations of the immune system.11
The Neuroendocrine System and Gene Regulation are Complex Too
The neuroendocrine system and gene regulation are important controls of homeostasis that are positively affected by whole-body thermotherapy. The physiology has been studied since the 1990s.
Cancer research is showing there is a close link between increases in body temperature and gene regulation. At least 120 small sections of our genes (microRNAs) are affected by high body temperatures.12 This study was of only one type of cell and the authors suggest that cells from other parts of the body may react differently to heat stress. So while some genetic code is regulated by heating, many other RNA segments are involved in doing the regulating.13
Little research has gone into the role of genetics in heat stress, but this area promises to be valuable in the treatment of cancer.14
The neuroendocrine system is found in almost every part of the body but especially in the gastrointestinal tract, the thyroid and lungs. Neuroendocrine cells are multitaskers, they act like nerve cells because they receive signals from nerves and also make hormones. During hyperthermia, the hypothalamic-pituitary-adrenal (HPA) axis, a major part of the neuroendocrine system, is stimulated. Endorphins, morphine-like substances, are produced by the hypothalamus and the pituitary gland. The pituitary gland also produces adrenocorticotropic hormone (ACTH), which stimulates the adrenal glands to release cortisol, an anti-inflammatory hormone.
This process begins when the sympathetic nervous system detects a rise in the body’s temperature and signals the adrenal glands to release dopamine, norepinephrine and epinephrine which stimulate the hypothalamus.15
Sauna can increase levels of cortisol
So something as simple as sauna will increase levels of cortisol, ACTH, epinephrine, norepinephrine and the fatigue hormone, prolactin (from the pituitary). Interestingly these levels are greater in women than in men.16 Just keeping the face cool during hyperthermia reduces the heart rate and prolactin levels.17
Research on the neuroendocrine system has been done mostly on healthy young people. Neuroendocrine and HPA axis dysregulation is common in chronic disease, so more research needs to be done to see if effects are different in ill people.15 This problem of studying the healthy, not those with a disease, applies to all the areas discussed on this page. Much of the research has been done on animals, or even isolated cells. Personally, I think responses to treatment will be quite different in people with conditions such as acute infections, diabetes, autoimmune and chronic heart disease.
You may be thinking that any increase in stress hormones is dangerous, or that it would be better if thermotherapy reduced the levels.
Well, it’s complicated!
Thermotherapy has recently been called a “hormetic strategy.”15 Hormesis is where just the right dose of therapy is beneficial while a lower, or especially a higher dose, is harmful. If thermotherapy is hometic, and I think it is, then all we have to do is find “just the right dose” of heat, or cold to treat your problem. No more and no less.
Surprisingly, that “dose” is relatively easy to find. If you have read this far, you realise that thermotherapy impacts many body processes in intimate and convoluted ways. How do we treat people safely while taking all this into account? And find that perfect dose?
Come with me to the next post, The Physiology is Complex, the Thermotherapy is Simple, where I’ll explain everything.
References:
- Sinclair M. Hydrotherapy for Bodyworkers: Improving Outcomes With Water Therapies. 2nd ed. Handspring Publishing Limited; 2020.
- Brinkman JE, Dorius B, Sharma S. Physiology, Body Fluids. In: StatPearls. StatPearls Publishing; 2020.
- Ray L, Iliff JJ, Heys JJ. Analysis of convective and diffusive transport in the brain interstitium. Fluids Barriers CNS. 2019;16(1):6.
- Eckhouse SR, Spinale FG. Changes in the myocardial interstitium and contribution to the progression of heart failure. Heart Fail Clin. 2012;8(1):7-20.
- Kuhlenhoelter AM, Kim K, Neff D, et al. Heat therapy promotes the expression of angiogenic regulators in human skeletal muscle. Am J Physiol Regul Integr Comp Physiol. 2016;311(2):R377-R391.
- Blum N, Blum A. Beneficial effects of sauna bathing for heart failure patients. Exp Clin Cardiol. 2007;12(1):29-32.
- Cohen M. Turning up the heat on COVID-19: heat as a therapeutic intervention. F1000Res. 2020;9:292.
- Brenner IK, Castellani JW, Gabaree C, et al. Immune changes in humans during cold exposure: effects of prior heating and exercise. J Appl Physiol. 1999;87(2). doi:10.1152/jappl.1999.87.2.
699 - Tian W, Zhang N, Jin R, et al. Immune suppression in the early stage of COVID-19 disease. Nat Commun. 2020;11(1):5859.
- Datta NR, Kok HP, Crezee H, Gaipl US, Bodis S. Integrating Loco-Regional Hyperthermia Into the Current Oncology Practice: SWOT and TOWS Analyses. Front Oncol. 2020;10:819.
- Frey B, Weiss E-M, Rubner Y, et al. Old and new facts about hyperthermia-induced modulations of the immune system. Int J Hyperthermia. 2012;28(6):528-542.
- Wilmink GJ, Roth CL, Ibey BL, et al. Identification of microRNAs associated with hyperthermia-induced cellular stress response. Cell Stress Chaperones. 2010;15(6):1027-1038.
- Place RF, Noonan EJ. Non-coding RNAs turn up the heat: an emerging layer of novel regulators in the mammalian heat shock response. Cell Stress Chaperones. 2014;19(2):159-172.
- Roufayel R, Kadry S. MicroRNAs: Crucial Regulators of Stress. Microrna. 2020;9(2):93-100.
- Gálvez I, Torres-Piles S, Ortega-Rincón E. Balneotherapy, Immune System, and Stress Response: A Hormetic Strategy? Int J Mol Sci. 2018;19(6). doi:10.3390/ijms19061687
- Jezová D, Kvetnanský R, Vigas M. Sex differences in endocrine response to hyperthermia in sauna. Acta Physiol Scand. 1994;150(3):293-298.
- Mündel T, Bunn SJ, Hooper PL, Jones DA. The effects of face cooling during hyperthermic exercise in man: evidence for an integrated thermal, neuroendocrine and behavioural response. Exp Physiol. 2007;92(1):187-195.
 AUTHOR
AUTHOR
BRUCE THOMPSON
BAppSc-Physiotherapy, Sydney University 1978
Bruce Thompson is a qualified Physiotherapist who has been using and teaching hydrotherapy for over 30 years.
See also:
traditionalhydrotherapy.com
hydro4covid.com



Leave A Comment